Medical billing is one of the most vital yet frequently overlooked aspects of healthcare operation, especially for medical practices in the USA. Indeed, minor miscalculations in the billing process can have a huge impact on profit, compliance, and patient satisfaction. Inaccurate billing can affect denied claims, delayed payments, or fiscal losses for your practice. In this companion, we’ll dive into the most common medical billing errors, explain their impact, and offer practical tips for doctors to effectively avoid these miscalculations.
Understanding the Common Medical Billing Errors
Billing errors in healthcare are a significant challenge for many medical practices. From minor clerical mistakes to more serious oversights, medical billing errors can have major repercussions. Below are the most common errors doctors and healthcare providers face when handling medical billing.

1. Incorrect Patient Information
One of the most frequent billing errors occurs when patient information is inaccurate. This includes details like the case’s name, date of birth, insurance details, and contact information. When these details are incorrect or mismatched, insurance companies may reject claims or detention payments.
Example: If a case’s insurance policy is listed under the wrong insurance provider or the date of birth is entered incorrectly, the claim will probably be denied, leading to payment detainments.
2. Coding Errors
Medical billing involves using specific codes to describe the procedures, services, or treatments provided. These codes, such as ICD-10 or CPT codes, must be accurate to ensure proper reimbursement. If these codes are outdated, incorrect, or mismatched, it can result in claim denials or even audits.
Example: Incorrectly coding a procedure as a more expensive treatment than it was actually performed can lead to overpayment, while undercoding may result in underpayment for the services rendered.
3. Duplicate Billing
Duplicate billing occurs when a claim is submitted further than formerly for the same service or procedure. This can be either by accident or due to poor billing practices. Not only can this spark an inspection, but it can also lead to penalties and prepayment demands.
Example: Submitting the same claim multiple times for the same office visit or procedure can flag the system and affect the healthcare provider being investigated.
4. Missing or Incomplete Documentation
Medical billing requires sufficient attestation to justify the procedures or treatments that were handed. Missing or deficient attestation can affect claim denials because insurance companies bear evidence of services rendered.
Example: If a procedure is billed, but the doctor’s notes do n’t include the necessary details about the case’s condition or the reason for the procedure, the insurance provider may reject the claim.
5. Incorrect Charge Entry
An incorrect charge entry happens when the charges for services, medications, or procedures are inaptly entered into the billing system. Whether due to typographical errors or misreading of the pricing system, incorrect charges can lead to billing disagreement.
Example: If a healthcare provider accidentally charges for an expensive procedure that wasn’t performed, the patient or insurance provider may overpay, leading to future claims being scrutinized.
How to Correct Medical Billing Errors Effectively
Correcting medical billing errors is a visionary process that involves careful attention to detail and a well- structured workflow. Below are some effective ways to correct medical billing errors and help them from passing again.
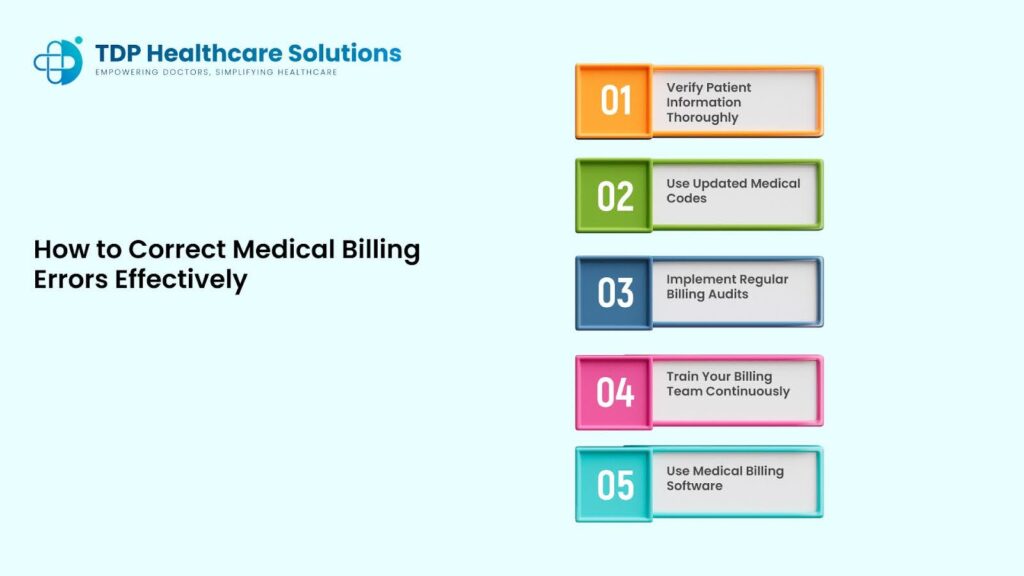
1. Verify Patient Information Thoroughly
Before submitting any claim, it’s pivotal to ensure the patient’s information is accurate. This includes checking the patient’s name, date of birth, insurance plan, and contact information. You should also confirm that the information is harmonious across all documents and insurance forms.
Tip: Always corroborate patient details at each visit and double- check insurance cards, as indeed the lowest distinction can beget billing errors.
2. Use Updated Medical Codes
Coding is at the core of medical billing. Medical codes( like ICD-10 for diagnoses or CPT for procedures) need to be current and accurate. Failure to use the rearmost codes can affect claim denials. Regularly modernize your coding coffers and ensure your billing staff is trained to apply the correct codes.
Tip: Schedule regular training sessions for your billing team to ensure they’re familiar with the rearmost coding systems and industry changes also, you can verify your ICD-10 Code on ICD10Data.
3. Implement Regular Billing Audits
Periodic internal audits are an effective way to identify recurring errors before they escalate. By regularly reviewing submitted claims, you can spot patterns and pinpoint areas where mistakes are most common.
Tip: Use audit tools to cross-check claims against industry standards and identify discrepancies early on.
4. Train Your Billing Team Continuously
Billing and coding procedures are constantly evolving due to updates in insurance regulations and medical practices. To avoid crimes, it’s essential to train your billing platoon constantly. Training should cover everything from proper attestation ways to the rearmost rendering updates.
Tip: Encourage your staff to attend webinars, shops, and certifications to stay on top of the rearmost stylish practices in medical billing.
5. Use Medical Billing Software
Implementing advanced medical billing software can drastically reduce errors. Many billing software programs have built-in features to check for errors before a claim is submitted. This includes automatic checks for accurate codes, patient details, and payment tracking.
Tip: Invest in billing software with automated claim scrubbing features, which review claims for errors before submission to insurance providers.
Best Practices for Avoiding Common Billing Errors in Healthcare
Minimizing medical billing errors does not just depend on addressing issues when they arise; it requires enforcing stylish practices that reduce the liability of crimes from the launch. These practices help streamline workflows and improve delicacy across the billing process.
Establish Standard Operating Procedures (SOPs)
Standard Operating Procedures( SOPs) should be created for all stages of the billing process. From authenticating patient data to submitting claims, SOPs ensure that every step is completed rightly and constantly.
Tip: Regularly review and modernize your SOPs to keep them in line with changing assiduity regulations.
Maintain Regular Communication with Insurance Providers
Regularly communicate with insurance companies to ensure you are over to date on policy changes, claims requirements, and other applicable details. Being apprehensive of insurer-specific billing preferences or updates can save your practice time and money.
Tip: Set up recreating meetings with insurance representatives or use digital tools to stay informed about any changes in billing requirements.
Use Automated Claim Scrubbing Tools
Automated claim scrubbing tools can help detect errors in medical billing before claims are submitted. These tools scan the claim for coding issues, missing documentation, or other inconsistencies that could lead to denials.
Tip: Consider using a medical billing software that integrates with claim scrubbing tools for more efficient error correction.
Impact of Medical Billing Errors on Medical Practices
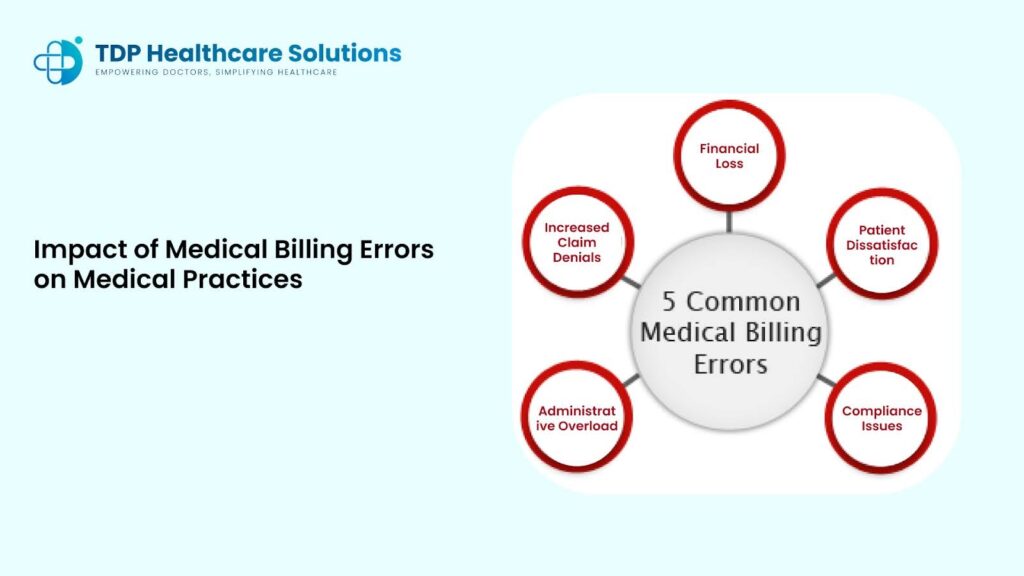
When billing errors go unaddressed, they can create ripple effects that affect both the financial and operational health of a practice. These impacts include:
- Increased Claim Denials: Errors result in a higher volume of denied claims, which can negatively affect your practice’s revenue.
- Financial Loss: If medical billing mistakes lead to underpayment or overpayment, your practice could lose out on substantial revenue.
- Patient Dissatisfaction: Billing errors can frustrate patients, particularly if they receive inaccurate bills or experience delays in processing payments.
- Compliance Issues: Incorrect billing practices may lead to compliance issues or legal problems, including penalties from regulatory bodies.
- Administrative Overload: Reworking denied or rejected claims creates additional work for staff, resulting in a higher administrative burden.
Conclusion:
At TDP Services, we understand the challenges that doctors and healthcare providers face when managing medical billing. By addressing the most common medical billing errors and enforcing visionary measures, healthcare practices can reduce the impact of these mistakes and improve their financial issues. The key is to stay informed, use the right tools, and develop harmonious workflows that minimize crimes. For expert medical billing support that’s acclimatized to your practice, don’t hesitate to communicate with us.
Frequently Asked Questions (FAQs)
1. What are the most common medical billing errors in healthcare?
Answer: The most frequent medical billing errors include incorrect patient information, coding errors, duplicate billing, and incomplete documentation.
2. How can doctors avoid billing errors?
Answer: Doctors can avoid billing errors by arguing patient data at each visit, staying streamlined on coding norms, training staff regularly, and using medical billing software to streamline the process.
3. What happens if medical billing errors are not fixed?
Answer: Unresolved billing errors can lead to claim denials, financial losses, audits, and damage to patient trust, negatively impacting a practice’s reputation and financial health.
4. How does medical billing software help in reducing errors?
Answer: Medical billing software helps reduce errors by providing automated checks, real-time validation of codes, and alerts for missing or incorrect data, ensuring the submission of accurate claims.
5. Can outsourcing medical billing services help reduce errors?
Answer: Yes, outsourcing medical billing services to experienced providers ensures that billing is handled by experts, reducing errors, improving compliance, and speeding up the claim process.